Israel Sarrió arrived at the Rehabilitation Center of Levante from Hospital Peset in Valencia (Spain) on January 31st of 2004 with an amputation of the left arm 2 inches above the elbow.



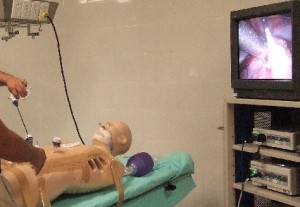
Click on images for large sizeAt 14:00hrs, the microsurgery implant began. The first maneuver consisted in lavage and sterilization of the amputated arm and its connection to the brachial artery by a silicone tube in order to revascularize it.
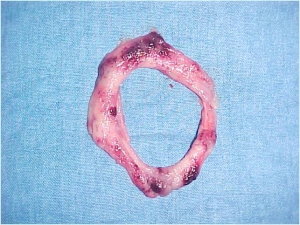
Later we rebuilt the humerus and repaired the brachial artery, the basilic and cephalic veins, and the three nerves of the arm.
This proccess lasted 21 hours, and the reimplantation was successful. The patient went to the Intensive Care Unit during that night and the next day, he went to a normal room.

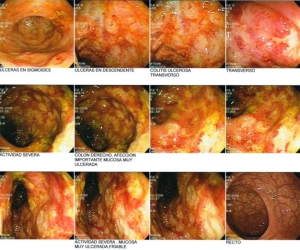
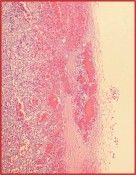
Two days later, we found a wound infection that was seriously compromising the viability of the reimplantation. We talked to the family and they told us that the day of the accident the arm fell in a drain. This contamination was the probable cause of the unfavorable progress. The situation was critical, and we said to the family that there were two different options: reamputate the arm or try to save it by taking it into a healthy zone where it would be possible to nourish it while we cleaned the infected area.

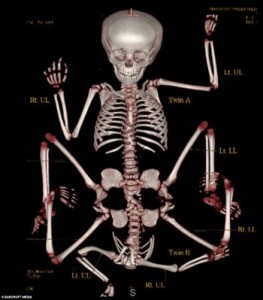
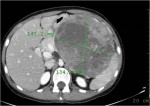
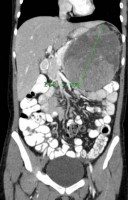
The idea of taking the arm to another anatomical location came by reading a similar case published by Michael Wood (Mayo Clinic, Rochester, MN, USA) in which he attached an arm in the groin. The uniqueness of our case consisted of using the procedure to rescue the limb from an infection, called a Deferred Transitory Heterotopic Implant. This was the first such case of involving an elbow.
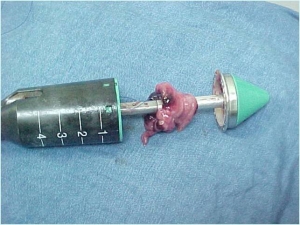
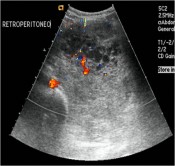
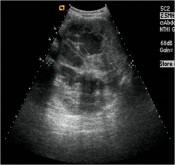
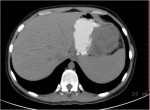
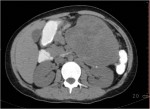
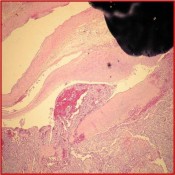
With the agreement of the family it was decided to transfer the arm to the groin where large blood vessels are readily accessible. In 4 hours we disassembled the reconstruction performed earlier and connected the blood vessels of the arm to those of groin by means of microsurgery.




The psychological impact on the patient was very important. As soon as he woke up, we told him that the arm was infected and we have to save it in other location on his body. After a couple of hours he realized that the arm was on his leg. He stayed that way for nine days with daily cleanings until it was verified that the stump was clean.
On February 12nd of 2004, we reimplanted the arm in its original place, rebuilding bone, arteries, veins, nerves, muscles and skin in a procedure of 6 hours.


Afterwards, the patient was doing physically and psychologically well, happy that he have not have to lose his arm.
By this time the patient could move his elbow. From the time of the surgery, the repaired nerve functionality is growing at a speed of 1 milimeter per day. In about 6 months we hope that he will be able to move his hand and fingers.
The function which we hoped to obtain from this procedure was better than those obtained with an amputation and the prosthesis. The patient will be able to grasp objects, to perform normal life functions, such as tie his shoes, all with small orthopedic aids.

The complete surgical team of the Unit of Hand and Reconstructive Surgery was involved in this operation, with Dr. Pedro Cavadas leading the team, and Dr. Navarro, Dr. Soler, Dr. Duke and Dr. Landin as assistants.
Via